Healthcare workers are the front-line COVID-19 response team, indisputably essential to containing this unpredictable, highly lethal and significantly consequential pandemic. Unlike their aviation counterparts who are supported through high stress situations, clinicians often lack two essential tools that are basics in the cockpit: real-time decision-support systems and daily reconnaissance. The Medical Brain was built for both and delivers the power of aviation tools to the clinical environment.
What Aviation Can Teach Us About Health Care And The COVID-19 Response
Having spent time in aviation, I’ve had the experience of dealing with the complexities of flight and the risk associated with hundreds of variables—known and unknown—threatening catastrophe if mishandled.
Despite this daunting risk equation, the industry’s safety record is remarkable. In 2019, for instance, nearly 3 million passengers flew across the US on a daily basis. They all landed safely.1
Unsurprisingly, there are parallels between the aviation and health care industries. Both share complexities of similar magnitude, and both have high stakes—life and death, in fact—should errors occur.
In the wake of the COVID-19 pandemic and the stressors it has placed on health care systems and professionals worldwide, let’s take a look at how health care can learn a thing or two from aviation.
We didn’t handle COVID-19 the same way we handle flight risks
The immense pressure and emotional toll COVID-19 has had on our health care professionals. As with highly complex flight missions, COVID-19 proved to be a complex, demanding, and stressful challenge—one that we knew would have dire consequences if not successfully controlled.
While dwelling on what could have been is not the best way forward, I believe that addressing the multivariate, unpredictable nature of the pandemic in the same way we manage flight risks could have positively impacted the lives of millions of Americans.
How aviation systems support decision-making
During my many years in aviation, I became intimately acquainted with numerous systems whose sole purpose was to control flight outcomes by controlling for human error.
The airline industry leverages data from all possible sources, delivers it at the precise time needed in an easy to digest format, creating an exacting culture of hazard control.
Although skilled and highly trained professionals are essential to the aviation and health care industries, human error is always a risk. It’s a risk that has significant emotional consequences for pilots and clinicians alike, who rightly demand professional excellence of themselves.
The use of real-time, intelligent support systems is designed to mitigate these risks. Such tools, along with daily reconnaissance and strict protocols, allow pilots to make instantaneous adjustments and ensure that errors which could complicate flight performance are rapidly addressed. This kind of systemic due diligence gives pilots and passengers peace of mind.
What I saw in my aviation days were systems that presented only the most critical elements needed for each moment of a flight in a precise, easy-to-understand display. There was no hunting through multiple screens or sifting through extraneous data points to find the essential elements needed at any given moment.
Thanks to this simplicity and ease of use, pilots are able to perform their duties with exacting precision even in the most intense, unpredictable situations—like those clinicians are facing on a daily basis with the COVID-19 crisis.
Health care lacks these mission-critical support systems
In my early 30s, I became a physician. And I quickly realized just how different health care was from my previous line of work.
At the time, the healthcare industry was lagging behind aviation when it came to maintaining a high degree of performance under extreme circumstances. Critical patient information was and still is often scattered across disconnected records and buried in isolated archives.
Health care and aviation are two professions that deal with equally high stakes—life and death—yet use completely different tools to handle them. Not enough attention has been paid to providing health care professionals with intelligent, well-integrated support systems—systems that would help them manage the extreme complexity and stress, especially that which we are experiencing with COVID-19.
The birth of the Medical Brain
Ultimately, I left my clinical practice. But the vast, gaping chasm between aviation technology and healthcare technology stuck with me.
I have spent much of my professional life bridging that gap by placing data-driven decision-support tools in the hands of clinicians and consumers. Our vision at healthPrecision was to create an intelligent digital platform that links all data sources and combs through them to form an accurate, updated picture of any clinical situation.
This vision led to the conception of Medical Brain—a tool built with artificial intelligence, machine learning, and extensive medical expertise.
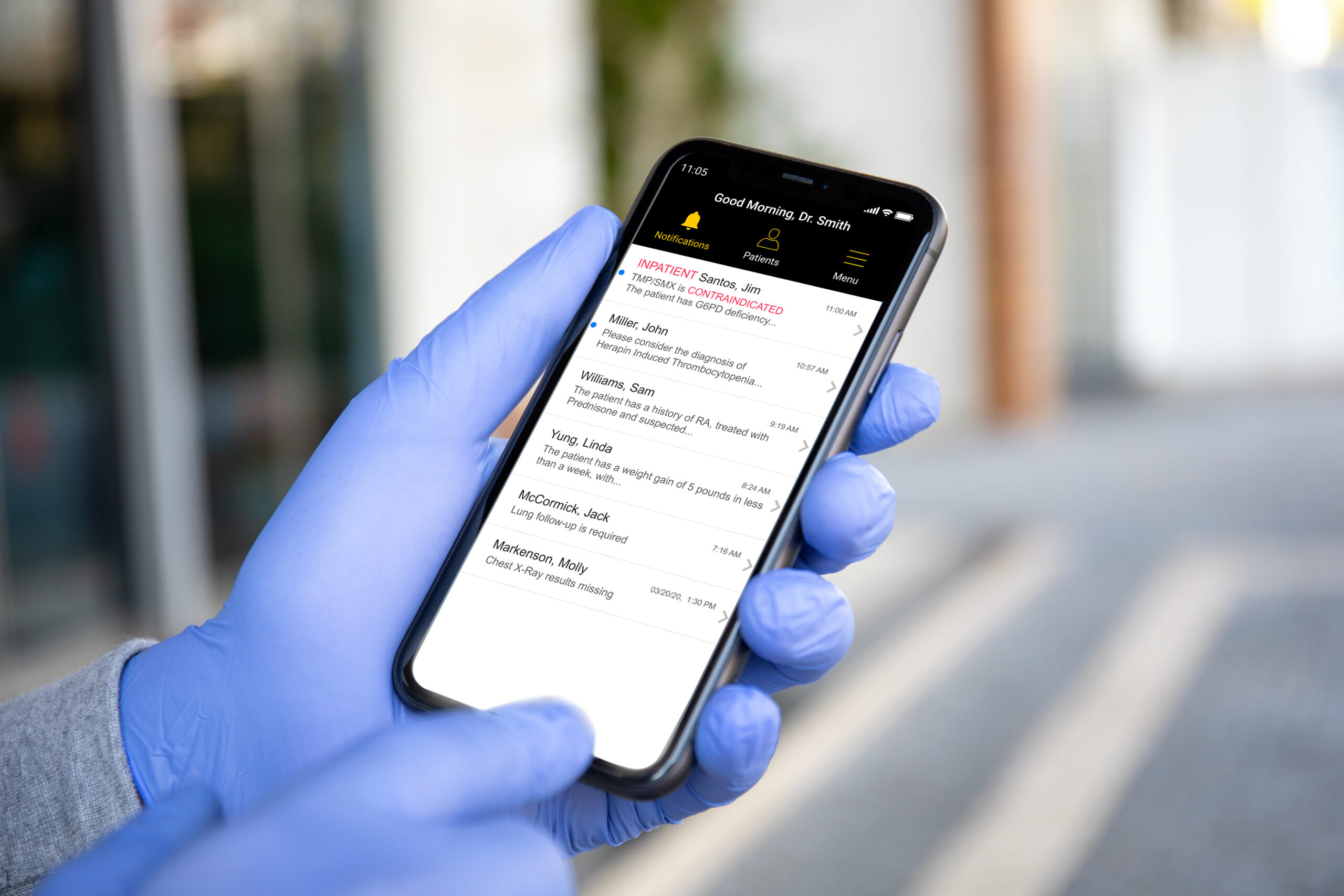
Medical Brain actively searches all data sources, including EHRs and analyzes critical information often buried in free text, to identify health deterioration risks as well as gaps and errors in care. When detected, it notifies clinicians and patients and coordinates actions to remediate the situation.
Our focus on health care quality was inspired by my time in aviation. The aim is to reduce measurable “never” events—errors that are strongly associated with negative outcomes. These errors are very common in health care due to the industry’s high dependency on human work, which is deeply embedded in clinical processes.
Medical Brain has been in use over the last few years in acute and ambulatory care settings, helping providers and their patients navigate high-risk situations. By maintaining aviation-level quality (with alerts specificity >95% as our standard), busy clinicians have experienced lower alert fatigue and higher levels of clinical protocol compliance.
Thanks to this approach, significant reductions in “never” events have been achieved, in some places reaching >90% sustained reduction measured in regular reconnaissance analysis.
And then along came COVID-19…
The COVID-19 pandemic presented an unprecedented opportunity to utilize Medical Brain’s capabilities and performance.
Working together with our health care clients, we examined predicted hazards and considered multiple factors: excessive workforce stress, system and capacity shortages, and uncharted scientific territories.
First and foremost, we were asked to assist health care providers in performing their extraordinarily difficult jobs by embedding continuously updated COVID-19 content in the Medical Brain. In New York City, the original epicenter of the disease, we were asked to assist hospitals as well as public health and government employees.
Today, thousands of health care employees are communicating on a daily basis with the Medical Brain. It assists in determining COVID-19 risks based on accurate differential diagnosis—taking into account underlying health conditions, multivariate symptom analysis, and COVID-19 exposure—to determine if an employee would qualify to report to work, or if they might require home isolation and medical support.
Artificial (and emotional) intelligence matters
With the safety of health care workers and their families weighing heavily on their minds, provider stress levels reached an all-time high during the height of the COVID-19 pandemic.2 , 3 , 4 , 5, 6, 7 We at healthPrecision saw a unique opportunity to provide the additional support needed to see providers through these unforeseen circumstances.
Placing reliable systems in the hands of clinicians has helped them deal with the stressors of an unknown, novel pandemic. Medical Brain acted as a control mechanism that helped clinicians maintain quality and mitigate risks so they could focus more on protecting patients. This is due in no small part to the sheer power and capacity of AI decision support.
An emotional support engine was also added to Medical Brain, offering on-demand conversation, coping support, and as-needed referrals. As always, rapid accuracy was the deciding factor in achieving user confidence and long-term stable adoption of this tool.
Clinicians are pilots, too
When pilots complete intense missions, reconnaissance closes the loop for risk control.
As James Fallows notes in his brilliant article recently published in The Atlantic, ‘‘Aviation is safe in large part because it learns from its disasters.’’ He asks, ‘‘How would this look in an NTSB [National Transportation Safety Board] report?’’ He was referring to a post-pandemic review that most likely would never happen.8
Our ultimate aim at healthPrecision is to keep our workforce healthy and functioning at the levels required to control the COVID-19 pandemic by continuously supporting their physical, emotional, and professional practice needs.
We strive to achieve this by providing the healthcare industry with tools that possess the same level of intelligence and capability as those used in a precision-driven industry like aviation.
In the end, we still have much to learn from our experiences with this pandemic. Our health care professionals—and the patients we serve—deserve better.
Sources
- Federal Aviation Administration. Air traffic by the numbers. 2020. https://www.faa.gov/air_traffic/by_the_numbers/. Accessed July 7, 2020.
- Hoffman J. ‘I can’t turn my brain off’: PTSD and burnout threaten medical workers. New York Times. 2020. https://www.nytimes.com/2020/05/16/health/coronavirus-ptsd-medical-workers.html. Accessed July 7, 2020.
- Dreifuss BA. I’m a health care worker. You need to know how close we are to breaking. 2020. https://www.nytimes.com/2020/06/26/opinion/coronavirus-arizone-hospitals.html. Accessed July 7, 2020.
- Law T. ‘We carry that burden.’ Medical workers fighting COVID-19 are facing a mental health crisis. 2020. https://time.com/5817435/covid-19-mental-health-coronavirus/. Accessed July 7, 2020.
- Stuart JC. Making the call. N Engl J Med 2020;383:e46.
- Dzau VJ, Kirch D, Nasca T. Preventing a parallel pandemic—a national strategy to protect clinical well-being. N Engl J Med 2020;383:513–515.
- Adams JG, Walls RM. Supporting the health care workforce during the COVID-19 global epidemic. JAMA 2020;323:1439–1440.
- Fallows J. The 3 weeks that changed everything. The Atlantic. 2020. https://www.theatlantic.com/politics/archive/2020/06/how-white-house-coronavirus-response-went-wrong/613591/. Accessed July 7, 2020.